Pancuronium bromide: Pharmacology, ADME properties and Side-effects
May 21,2025
Introduction
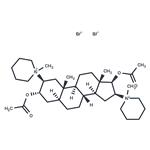
Pancuronium bromide (Figure 1) is an aminosteriod, consisting of quaternary ammonium and ester groups incorporated in asteriod base. It is an odorless, white crystalline powder compatible for solution with 5% dextrose in water, 5% dextrose in saline. Ringer's lactate solution, and normal saline in either glass or plastic containers. Because of its steroidal structure, pancuronium bromide may be absorbed into plastic containers during prolonged contact. Pancuronium bromide is a competitive, nondepolarizing neuromuscular blocking agent whose predominate pharmacologic action is at the postjunctional neuromuscular receptor site for acetylcholine.

Pharmacology
Several studies also show it decreases the prejunctional release of acetylcholine. The larger the intravenous dose, the shorter the interval before onset of neuromuscular blockade. Given intravenously, 0,04 mg/kg body weight of pancuronium bromide begins to depress neuromuscular transmission in 43±6 sec and reaches its peak effect in 236±12 sec. It is approximately five to 10 times more potent on a milligram-per-kilogram basis than d-tubocurarine, but it does not release histamine asdoes d-tubocurarine. Given in multiple doses, each succeeding dose of pancuronium bromide only marginally increases the magnitude of electrically induced muscle twitch depression, but significantly extends its duration of activity. Human studies of pancuronium bromidehave established that it causes moderate increases in heart rate with an attendant increase in cardiac output and blood pressure; there is no measurable effect on systemic vascular resistance. These effects have been variably attributed to a vagolytic effect, an indirect or a direct sympathomimetic effect. After pretreating patients with atropine, subsequent administration of pancuronium bromide results in no further cardiovascular alterations. Pancuronium bromide blocks the negative chronotropic and inotropic actions of cholinergic agents in anesthetized dogs; it does not affect the cardiac response to potassium chloride, which indicates that it selectively blocks the muscarinic cholinergic receptors of the heart. On the other hand, pancuronium bromide has indirect sympathomimetic actions. Pancuronium bromide probably releases adrenergic transmitters from postganglionic nerve endings.
It has no known effects on intraocular, intracranial, or intra-abdominal pressure, nor does it have a direct effect on the electroencephalogram. Despite its steroidal structure, the drug exhibits no known hormonal activity. Pancuronium bromide is antagonized by acetylcholine, anticholinesterase, potassium, and calcium. Its neuromuscular blocking action is increased by inhalation anesthetics, quinine, quinidine, magnesium salts, hypokalemia, lithium carbonate, and certain antibiotics such as neomycin, streptomycin, kanamycin, bacitracin, polymyxin-B, gentamicin, colistin,viomycin, lincomycin, clindamycin, and tetracycline as well as large doses of sedative hypnotics and barbiturates. Narcotics do not potentiate the neuromuscular block of pancuronium bromide.[1]
Absorption, Distribution, Metabolism, and Excretion
In humans, pancuronium bromide's concentration in plasma falls rapidly, in three phases. After a 6 mg intravenous injection in individuals weighing 70 kg, 60% of the drug disappears in less than 5 min, 80% after 30 min,and approximately 90% after 1 h. The rapid equilibration between plasma and extracellular fluid accounts for the rapid onset of neuromuscular blocking activity. Protein binding of pancuronium bromide does not appear to be significant. Patients with hypoalbuminemia or hypogammaglobinemia respond normally to the drug. In cats, fluorometric assay of liver and kidney homogenates 8 h after administration showed 24% of an injected dose in the liver and 1% in the kidneys. This amount, together with the drug recovered from the urine (30%) and bile (24%), accounts for about 80% of the dose administered. The drug is eliminated primarily unchanged by the kidneys, although a small fraction may be metabolized.Some of the unchanged drug may be eliminated in bile.In the cat approximately 80% of the drug is excreted unchanged, and the remainder is excreted in the form of metabolites. The major metabolite is a three hydroxy-derivative, probably the result of deacetylization by hepatic microsomal enzymes. [2,3]
During hepatic failure there may be an alteration induration of muscle relaxation after pancuronium bromide's administration. In one study, duration of neuromuscular blockade was shorter in patients with liver disease compared with those with normal liver function (an average of 18.5 min versus 47 min), but others have reported no apparent effect of liver disease on either the potency or duration of neuromuscular blockade after administration of pancuronium bromide.There is a wide variation in individual patient response to muscle relaxants. Even when standardization of experimental techniques has been meticulously employed, a marked variation persists both in vivo and in vitro. Some patients have greater than 90% neuromuscular blockade after 0.02 mg/kg body weight of pancuronium bromide administered intravenously, whereas the same dose given to other patients produced no detectable block.[4]
Side-effects
Side-effects from the use of pancuronium bromide are rare. Local signs of histamine release such as erythema or skin rash, as well as burning along the vein and increased pharyngeal and tracheal secretions have been encountered rarely. As pancuronium bromide has little cardiovascular and no bronchoconstrictor activity, it has been used without complication in 'poor risk' patients, including those suffering from cardiac disease, bronchial asthma or allergic diatheses. Pancuronium bromide has also been used in patients with hepatic or renal disease and inpatients on high corticosteroid dosage without untoward effects. However, patients with hepatic disease may require larger doses of pancuronium bromide than patients with normal liver function, and in patients with renal insufficiency prolonged relaxation or apparent recurarisation may occur.[5]
References
[1]Roizen MF, Feeley TW. Pancuronium bromide. Ann Intern Med. 1978;88(1):64-68. doi:10.7326/0003-4819-88-1-64
[2]Agoston S, Vermeer GA, Kertsten UW, Meijer DK. The fate of pancuronium bromide in man. Acta Anaesthesiol Scand. 1973;17(4):267-275. doi:10.1111/j.1399-6576.1973.tb00839.x
[3]Agoston S, Kersten UW, Meijer DK. The fate of pancuronium bromide in the cat. Acta Anaesthesiol Scand. 1973;17(2):129-135. doi:10.1111/j.1399-6576.1973.tb00807.x
[4]Katz RL. Clinical neuromuscular pharmacology of pancuronium. Anesthesiology. 1971;34(6):550-556. doi:10.1097/00000542-197106000-00015
[5]Speight TM, Avery GS. Pancuronium bromide: a review of its pharmacological properties and clinical application. Drugs. 1972;4(3):163-226. doi:10.2165/00003495-197204030-00002
- Related articles
- Related Qustion
- A muscle relaxant: Pancuronium bromide Mar 21, 2022
Pancuronium bromide, a muscle relaxant, is used primarily as a neuromuscular blocking agent to relax muscles during surgery. It is also used in some US states as the second ingredient in the three-drug injection sequence for administering
Supplementation with pyridoxal 5'-phosphate monohydrate can synthesize neurotransmitters such as dopamine and serotonin, maintaining a healthy nervous system.....
Nov 4,2025Biochemical EngineeringTerbutaline Sulfate, a synthetic beta-2 agonist since the late 1960s, is used for bronchospasm in respiratory diseases and has off-label uses.....
May 21,2025APIPancuronium bromide
15500-66-0You may like
Pancuronium bromide manufacturers
- Pancuronium bromide
-

- $0.00 / 1g
- 2025-12-18
- CAS:15500-66-0
- Min. Order: 1g
- Purity: 98%-102%
- Supply Ability: 1000g
- Pancuronium bromide
-

- $0.00 / 10mg
- 2025-12-16
- CAS:15500-66-0
- Min. Order: 10mg
- Purity: 98
- Supply Ability: 10000000
- Pancuronium dibromide
-
- $32.00 / 5mg
- 2025-12-10
- CAS:15500-66-0
- Min. Order:
- Purity: 99.86%
- Supply Ability: 10g